Read this Chiropractic Billing and Coding guide to find out:
- The basics of chiropractic medical billing and coding to save your valuable time and money.
- Challenges you may be facing in billing insurance companies and their solutions.
- Chiropractic insurance billing, clearinghouse, and insurance payers processes can help you be in control of cash flow.
- Steps for patient record documentation and billing automation that will put reimbursements in your pocket faster.
- Benefits of utilizing chiropractic billing services and chiropractic EHR and billing software.
“How do I maximize insurance reimbursement for every single patient that walks into my office?”
Do you have the same question in your mind?
Are you billing all you can? Are you using the correct chiropractic coding in your claims?
Spend a little time reading this guide to analyze whether you have the correct chiro billing strategies in place or not.
What is Chiropractic Insurance Billing?
Chiropractic care is included in most health insurance plans, but with certain limitations. Medicare, some Medicaid plans and companies like Blue Cross Blue Shield, United Healthcare, Aetna, and Cigna also provide chiropractic treatment coverage.
Accepting insurance at your chiropractic office offers patients the ability to pay for the cost of your chiropractic treatment. Becoming in-network with insurance companies can help you reach new clients. Patients who are covered by insurance prefer to go to a chiropractor who accepts insurance plans. Accepting insurance also increases patient loyalty.
Chiropractic insurance billing and coding is the process of getting paid for your chiropractic treatment services through the submission of insurance claims to the insurance carrier. You may have to send primary, secondary, and even tertiary insurance claims as well as patient records and statements to get full payment.
Chiropractic insurance billing is a time-intensive process. It requires precision. The smallest of errors can lead to unwanted losses. The problem with billing starts when your practice starts to grow. If you are an independent practice and manage all administrative work yourself, it becomes more difficult to keep up with all the required tasks of insurance billing, claim denial management, and monitoring reimbursements.
If you want to make sure you get paid for all your visits, you must have a good understanding of how to bill correctly, codes for each treatment type, and an automated chiropractic EHR and billing software system or utilize the professional expertise of chiropractor billing services to manage billing, claims, and collections all in one place.
Unlocking efficient chiropractic billing is crucial for any medical practice’s success. With the right resources and tools, navigating the complexities of billing becomes a breeze. Here, are the 8 Free Chiropractic Medical Billing Resources to streamline your billing processes
Chiropractic CPT Code Cheat Sheet
What Are Chiropractic CPT Codes
Chiropractic CPT codes are the codes for procedures performed by a provider during a patient visit.
Chiropractic CPT Codes for chiropractic services document the various diagnoses, procedures, and evaluations involving chiropractic treatments. CPT codes reflect what the provider would like to get reimbursement for from insurance payers. Since chiro billing codes are used to bill insurance companies, it is important to accurately document each diagnosis and associated CPT codes during invoicing.
What CPT codes can a chiropractor bill?
Current Procedural Terminology (CPT) codes for chiropractors have been created and maintained by the American Medical Association. These five alpha-numeric character chiropractic codes describe all of the evaluation, treatment, imaging, examinations, and diagnosis services rendered to patients by chiropractic practices for insurance purposes. Knowing and understanding the importance of CPT codes for chiropractic services are crucial as billing with incorrect chiropractic therapy CPT codes can lead to claim rejections and payment delays.
The CPT code set contains tens of thousands of codes for medical procedures. Other healthcare providers use a number of chiropractic codes, but chiropractors use only a limited set of CPT codes. There are four main codes that chiropractors use for billing manipulative treatment services:
CPT Code 98940 Chiropractic manipulative treatment (CMT); Spinal, 1-2 regions
CPT Code 98941 Chiropractic manipulative treatment (CMT); Spinal, 3-4 regions
CPT Code 98942 Chiropractic manipulative treatment (CMT); Spinal, 5 regions
CPT Code 98943 Chiropractic manipulative treatment (CMT); Extraspinal, 1 or more regions
Here is a list of the common chiropractic CPT codes used by practices in the US:
| 99202 | 97162 | 97112 |
| 99203 | 97535 | 97530 |
| 99204 | 97032 | 97010 |
| 99212 | 97012 | 97014 |
| 99213 | 97113 | 97035 |
| 99214 | 97124 | 97161 |
| 97140 | 97018 | 97116 |
| 97110 | 97022 | 97033 |
| 97750 | 97026 | 97039 |
| 99211 | 97014 | 97032 |
Tips for Chiropractic CPT Codes for Better Insurance Reimbursements
Stay up to date with code changes
Practicing chiropractors need to know almost as much about chiropractic billing codes as they do about their patients. CPT codes for chiropractic services are revised and updated throughout the year. Chiropractic practices need to stay updated and current with the chiropractic billing code changes. For instance, the CMS guideline for chiropractic billing and coding states that “The AT modifier must not be placed on the claim when maintenance therapy has been provided. Claims without the AT modifier will be considered as maintenance therapy and denied.” If your billing staff feels overwhelmed with the constantly changing insurance billing landscape, hiring chiropractor billing services will help you avoid claim denials or rejections due to coding errors or insufficient documentation.
Well-documented patient record
To ensure your practice follows a smooth insurance billing process, it is crucial to maintain well-documented patient charts and paperwork. From insurance records, and patient demographics to diagnoses and procedures performed, make sure you maintain an accurate patient record to get the maximum reimbursements for the services rendered. Use integrated EHR and chiropractic billing solutions to manage patient records and billing effectively.
CPT coding for mechanical traction versus CMT
CPT Code 97012 is used for coding mechanical traction, most often for the lumbar or cervical spine to relieve pain and improve tissue flexibility. Chiropractic Manipulative Treatment (CMT) codes (98940-98943) include a pre-manipulation patient assessment, the adjustment, and the evaluation of the effect of treatment. Based on the guidelines for chiropractic billing codes, CMT and mechanical traction should be used carefully when billing insurance companies. Some payers deny chiropractic CPT codes for billing Mechanical Traction services rendered on the same date of service as the CMT treatment. Before submitting your claims, you must know the chiropractic coding rules and requirements for different payers.
Analyze your billing reports and denials
Analyzing your billing reports will help you identify how much you’re being paid by payers for each chiropractic therapy CPT code. If you have denied claims, make sure to check what went wrong. Analyzing chiropractic CPT codes for billing in denied claims can help you find patterns that can be corrected in the future to prevent losses. However, when you outsource your chiropractor billing services to zHealth, you get access to verified professionals who will submit your claims on time to make continual cash flow and an assured increase in revenue and take care of your claim denials.
What are Chiropractic ICD-10 Codes?
The International Classification of Diseases, Tenth Revision, Clinical Modification (ICD -10- CM) codes help to determine which type of treatment a provider needs to offer and what needs to be addressed. Using valid chiropractic ICD-10 codes can facilitate accurate claims payments and support the medical necessity of the service. One of the most common chiropractic ICD-10 codes is the vertebral “subluxation.” It is the diagnosis that is used to justify the performance of a chiropractic manipulative treatment or an adjustment.
ICD-10 codes for chiropractors have seven characters, which represent Section, Body System, Root Operation, Body Region, Approach, Method and Qualifier.
- The first three characters denote the category. All ICD-10 codes for chiropractic treatment under the same category are related to conditions.
- The next three characters specify anatomical site and severity.
- The seventh character in ICD 10 chiropractic codes is used to denote encounters, including Initial Encounter, Subsequent Encounter, or Sequela.
Importance of ICD-10 Codes for Chiropractors
ICD-10 codes for chiropractic are the standard transaction code set used by providers for diagnostic purposes under the Health Insurance Portability and Accountability Act (HIPAA). The code set is used for finding health care statistics, quality outcomes, mortality statistics, and billing. Understanding and educating yourself and your staff on appropriate coding will result in fewer claim denials, spending less time spent with payers trying to justify your claims, and a higher revenue stream.
General Tips for Coding Chiropractic ICD-10 Codes Effectively
Find the most specific code
With tens of thousands of ICD-10 codes, it will be virtually impossible to memorize them all. If you’re using chiropractic billing software, it will be easier to locate the code by just typing the first few letters of the diagnosis. The software will auto-populate the relevant codes based on your entered letters. Review the auto-populated results to find the most specific ICD 10 codes for chiropractors.
Identify the highest specificity
Official guideline for chiropractic billing and coding requires ICD-10 coding to the highest degree of specificity. Chiropractic providers have an obligation to document conditions to the full extent of their knowledge of the patient’s health. When you hire managed billing services, professional coders will ensure that you have assigned and reported ICD-10 codes for chiropractic services with the highest degree of specificity.
Document Chiropractic Diagnosis Codes Supporting CPT Codes
Insurance companies pay for procedures (CPT codes), not chiropractic diagnosis codes. But ICD-10 codes for chiropractic should be used to support chiropractic therapy CPT codes. When billing CPT codes, a provider must connect or “point” the diagnosis to each procedure performed. Remember, the total number of diagnosis pointers per CPT code is limited to four.
Chiropractic Modifier Codes
In English, a modifier may describe the who, what, how, why, or where of a situation. Similarly, modifier codes help chiropractors to indicate that a service or procedure has been altered due to some specific or unusual circumstance, such as why that procedure was necessary, where the procedure was performed on the body, what other services you used to complete the procedure, and so on.
There are various chiropractic modifiers that chiropractors can use when reporting chiropractic services. The modifier code is added to the CPT code with a hyphen and not to the ICD 10 chiropractic codes. If your selected CPT code requires a modifier and you fail to include it, your claim will be rejected by the insurance company.
A Complete Guide to Chiropractic Billing
How do chiropractors bill insurance?
1. Requirements
Coding descriptions and instructions are provided and maintained by the American Medical Association’s (AMA) Current Procedural Terminology (CPT®), Healthcare Common Procedure Coding System (HCPCS) developed by the Centers for Medicare and Medicaid Services (CMS).
All chiropractic services must be performed by a licensed provider. If services are performed by your chiropractic assistants (CAs), massage therapists, or other unlicensed providers under your direct supervision by a licensed chiropractor are not eligible for reimbursement.
Chiropractic services are subject to current procedural coding edits. Chiropractors must use modifiers when deemed necessary for billing insurance companies. Please check the CPT codes and ICD 10 codes for chiropractic Medicare and other payers provided above.
To bill insurers and get proper reimbursements, you must establish medical necessity for any treatment you provide. Medical necessity is any treatment, service, or test required after patient diagnosis, which may be justified as reasonable or necessary based on evidence-based standards of chiropractic care. It should be noted that Medicare and private insurance companies have different criteria to determine whether a given procedure, treatment, service, or test is a medical necessity or not.
For instance, Medicare Part B (Medical Insurance) covers manual manipulation of the spine provided by a chiropractor if medically necessary to correct a subluxation. Medicare doesn’t cover some ICD 10 codes for chiropractic services or tests a chiropractor orders, including X-rays, massage therapy, and acupuncture.
2. Chiropractic Coverage
Chiropractic coverage includes evaluation and management (E&M) services, radiology, chiropractic manipulative treatment, and modalities and procedures according to the reimbursement policies of insurance companies and Medicare.
When you perform diagnostic imaging services to find more information regarding the patient in terms of diagnosis, prognosis, and therapy planning, you must provide documents to bill and receive reimbursement for the same.
3. Documentation of Patient Records
Complete documentation of your patient’s history, treatment plans, tests and services, and patient statements is an essential component of proper billing and getting timely reimbursements. You must follow the standards for documentation and chiropractic records:
As a chiropractic practice, you must establish and maintain a separate and accurate treatment record for each patient.
Each patient entry shall be dated and signed by you. Such records shall be legible to review by a reviewer or auditor.
Documentation requirements for initial visits:
- The patient’s case history: Document the primary complaint of your patient. Apart from the main symptoms he or she is facing, you must document the patient’s family history, significant illnesses, and medical conditions, past medical history, medical allergies, and adverse reactions.
- Description of the present illness: Mention detailed information regarding the present health problem the patient is facing, such as quality and character of symptoms, onset, duration, intensity, frequency, location, and radiation of symptoms, aggravating or relieving factors, prior interventions, treatments, and medications are taken, secondary complaints, and main symptoms that caused the patient to seek treatment.
- Evaluation of musculoskeletal/nervous system through physical examination: Evaluation through physical examination is necessary to identify if there is subluxation that requires intervention and treatment. Follow the PART criteria to document evaluation findings:
P: PAIN and tenderness. Observe, examine, and document the pain exhibits with information about the intensity, location, and quality. Mention percussion, palpation, or provocation, pain grading scale, or audio confirmation by the patient, or include a questionnaire to describe their pain.
A: ASYMMETRY or misalignment. You can observe or notice patient posture or analyze gait, describe the spinal misaligned vertebrae and symmetry, and use and attach x-ray, CAT scan, or MRI result to identify misalignments.
R: RANGE of Abnormal Motion. You must diagnose and document the patient’s range of motion and record your palpation findings observation in a section or segment.
T: TISSUE TONE, TEXTURE, or TEMPERATURE. Observe and examine the abnormality in the soft tissues of the body, such as signs of spasm, inflammation, swelling, temperature changes, hypertonicity, hypotonicity, tautness, rigidity, and more. Document the instrument used and the findings.
- Diagnosis: Chiropractors are reimbursed for their claims only when the primary diagnosis for a patient is found to be subluxation. The precise level of the subluxation must be specified by the doctor of chiropractic. The document for specifying subluxation in the patient’s record must include the number and area of the spine, the ilii with the sacrum as an area where the patient has a condition, and the subluxation ICD-10 code.
- Treatment plan: The treatment plan must include the recommended level of care, specific treatment goals, and objective measures that can determine the effectiveness of the treatment.
- Informed consent or terms of acceptance by the patient
- SOAP notes for each patient encounter (Subjective, Objective, Assessment, and Plan notes)
- Date of initial treatment
- Details of supportive procedures or therapies, when administered, dispensed, or prescribed
Documentation requirements for subsequent visits:
1. Patient History: Chief complaint, changes since the last visit, and review if relevant
2. Physical examination: Examination of the spinal area involved in the diagnosis, assessment of change in patient condition since the last visit, and evaluation of treatment effectiveness.
3. Documentation: Document any treatment given on the day of the visit.
Tip: Use a fully-integrated billing software and practice management software for chiropractic practices that helps you dictate SOAP notes, upload clinical summaries, store lab test reports, document patient history, and more. Chiropractic medical billing software will simplify and automate your process of patient charting, patient statements, and insurance billing, thus saving you time, money, and hassles. If you want to save time and hassles and increase your cash flow, it could be beneficial to hire one of the best chiropractic billing companies.
4. Billing the Insurance Company
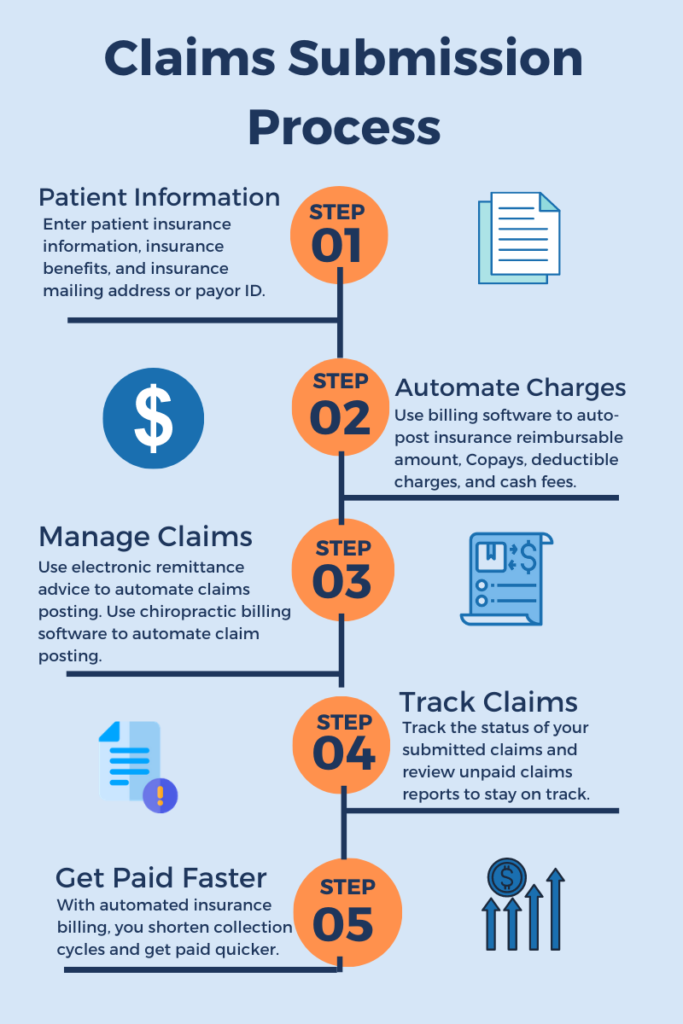
It’s easy to make mistakes when billing the insurance companies for each patient treatment and service. With the right coding and documentation, you can submit the claims easily and get reimbursed on time. Here are the steps involved in the reimbursement cycle:
- Check Eligibility: Checking eligibility prior to new patient appointment is the first step in the claim revenue cycle. Whether you have new patients or returning patients, find out if their insurance plans cover your chiropractic services.
- Patient Documentation: From appointment booking to generating an invoice for the chiropractic care you provide, every little detail should be documented properly. A single data entry mistake can mean claim denial. Although you can submit a corrected claim, why waste time and money when you can do it right away the first time? Electronic documentation and claims submission with chiropractic insurance billing software can improve the speed of your reimbursement cycle. Use chiropractic EHR software integrated with a billing tool and clearinghouse to make the billing process efficient.
- Utilize Managed Billing Services: With chiropractor billing services, you get expert help for managing your billing process with accurate ICD-10 coding, claim tracking, automated ERA posting & receiving, and more. Outsourcing chiropractor billing services can bring you bigger deals in gaining larger reimbursements. It helps you focus on your core competency, improve your revenue and have a smooth financial process.
- Timely File Claims: To avoid denials and get your reimbursements on time by meeting the timely filing deadlines. Also, by chiropractic insurance billing software, you can track the status of your claims. Generate Accounts Receivable reports to see where your money is, claims that are outstanding, and claim-related problems. Consider opting for a comprehensive all-in-one option that integrates your practice management system, EHR, billing, and more. By automating how you get paid, along with streamlining your other processes, you’ll have time to relax and get back to treating your patients.
Chiropractic Fees and Reimbursements Survey by Chiropractic Economics
Chiropractic Economics completed and published a web-based survey on fees and reimbursements in the US for the year 2022. When it comes to billings and collections, solo practices saw significant increases in both amounts this year. Solo DCs reported average billings of $429,800 and collections of $313,700, compared to average billings of $369,653 and collections of $263,737 last year.
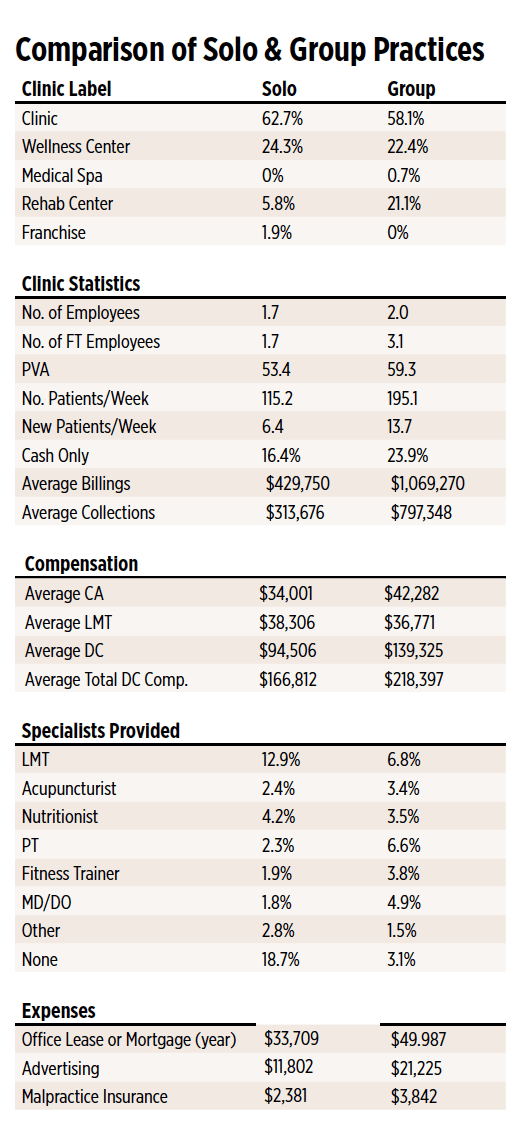
Image Source: Chiropractic Economics
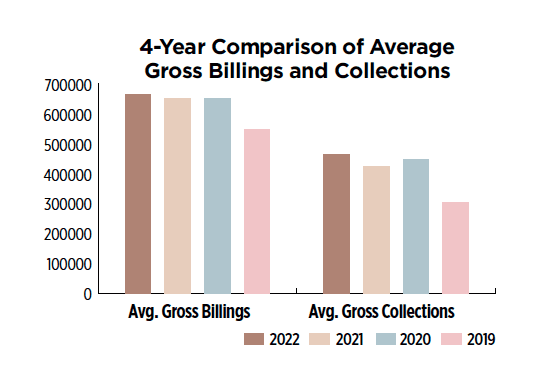
Image Source: Chiropractic Economics
Note: The survey by Chiropractic Economics is provided for informational purposes only. It is not intended to be used as a recommendation for setting fee levels or for getting reimbursed for chiropractic services or treatments.
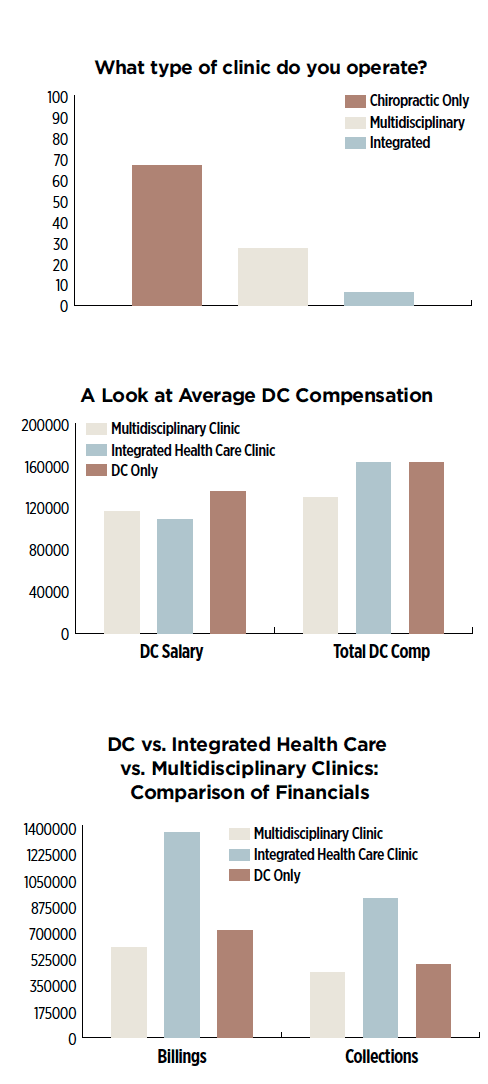
Image Source: Chiropractic Economics
In 2022, 65% of survey respondents reported offering chiropractic care only; 41% said they operated as a multidisciplinary clinic, significantly more than last year; and 30% responded as an integrated clinic. Integrated healthcare practices reported the highest billings ($1,400,000), while multidisciplinary practices reported billings of $715,000 and DC-only practices came in at $602,600.
Challenges in Chiropractic Billing and Coding
Some challenges in the billing and claims process are slow cash flow or revenue in the chiropractic industry. If you don’t have expert billers and coders or use chiropractic medical billing software, it will become a challenging task to increase revenue or grow your practice. Here are the billing challenges chiropractors face today:
1. Chiropractic Coding & Documentation
Chiropractors typically diagnose only a few types of muscle and joint conditions. Several factors such as CPT codes and chiropractic diagnosis codes linkage should be considered during chiropractic billing and even at the time of claims submission as well. Proper documentation to support medical necessity is very crucial and important for receiving claims reimbursement without rejections or denials.
2. Denials due to AR Management
One of the billing challenges that chiropractors face today is sloppy accounts receivables (AR) management. Often, the billing failure and the revenue drying up are because the facility fails to upgrade its AR management process. Since they depend on outdated software, they fail to match the evolving dynamics of the chiropractic billing regulations. Implementing chiro billing solutions could help in reducing AR and improve revenue.
3. Failure to Adhere to Payer Guidelines
Another significant challenge in billing that chiropractors face today is the varying levels of payer requirements such as:
- Medicare, Medicaid, or private health insurance plans have not authorized the procedure or are not covered under the plan.
- Some of the chiropractic services are not reimbursable.
- The level of reimbursement has exceeded.
In such cases, it is essential to take the help of chiropractic insurance billing services to ensure your claims are reimbursed quickly and timely.
4. Trailing Billings
Many times, chiropractic providers face the challenge of submitting claims on time. As a result, many try to catch up with the shortfalls. But in the long run, it leads to more complexities instead of increasing the revenue. With denials piling up and the billing department failing to follow up, the burden of the collection rate increases aggressively. The lack of data or proper reporting leads to further trailing in the billing and deteriorates the handling of the denials. With the best chiropractic billing services by your side, you don’t have to think about timely claim submissions, follow-ups, denials, or anything. You can take care of patients while the chiropractic medical billing services provider handles your billing complexities.
5. Untrained Staff
Most chiropractic practices are overburdened with work, and the failure to train and educate the staff on the new guidelines and documentation policies could result in incorrect billing and coding. It eventually leads to claim denials.
Solutions for Overcoming Billing Challenges
If your practice is not being managed efficiently, you are bound to experience issues with billing, patient experience, patient retention, and cash flow. Whether you’re billing an insurance company or the patient directly, you need to streamline your chiropractic practice to keep the money flowing in. Here are the tips you can follow to avoid delayed payments or claim denials:
- Use a robust chiropractic EHR system to obtain and record accurate patient demographics. Claims can be denied due to patient misidentification.
- Start using customizable, fully-integrated software for chiropractic billing services. Having all the information you need – from patient appointment details, and insurance information to SOAP notes and beyond – can help you reduce your stress, enhance patient management, promote accurate data entry, and efficient billing process.
- Instead of manually collecting payments each time a patient visits, use chiro medical billing software to submit auto-generated claims electronically. You will get much more time to focus on patients and growing your practice. zHealth Software is the most reliable chiropractic billing software that automates insurance reimbursement with auto-populated diagnosis coding on each SOAP note and provides real-time updates on the status of submitted claims.
- One of the best ways to overcome chiropractic billing challenges is to hire one of the best chiropractic billing companies. You need a partner who can provide end-to-end chiropractic billing solutions while optimizing the revenue cycle. zHealth offers the best chiropractic insurance billing services with a team of experts efficient in coding, documentation, AR management, follow-ups, denial management, and much more. A partner like us provides an integrated technology platform that helps you drive the business better with improved ROI.
- As your practice grows and you take on new patients, the billing issues increase, and you end up having to hire more people just to handle it all. zHealth chiropractic billing solutions power your practice with automated workflows, so your claims are submitted accurately and on time.
“I had never done my own billing before, but I have been doing it pretty seamlessly by myself since April when I started using zHealth chiropractic insurance billing software.”
The Step-by-Step Claim Submission Process
Benefits of Chiropractic Software for Insurance Billing Automation
Billing software for chiropractors is the core of your chiropractic practice. In today’s value-based care healthcare environment, the decision to utilize technology to support the billing process can have a long-lasting effect on the financial health of your practice. Consider using chiropractic insurance billing software. Why? Chiropractic medical billing software helps you get the best acceptance rates on your first submission, auto post ERAs, advanced claim scrubbing functionality, and automatic claim creation after you sign the SOAP note.
Using HIPAA-compliant chiropractic billing software that supports the in-house billing-claim-collections cycle management process is your best path forward. Even better, hiring one of the best chiropractic billing companies saves you tons of time and hassles while increasing revenue. Chiropractic medical billing services providers stay on top of their game with the latest knowledge of the coding rules and regulation changes by insurance companies. So you can submit accurate claims in a timely manner and get full reimbursements.
zHealth software automates your documentation process, insurance billing, and claims processing workflow.
- zHealth’s online patient check-in feature allows patients to fill in their information online with all submitted information going directly into the electronic health record system. zHealth Software has an integrated billing system. You save a lot of time and avoid making mistakes by automating the patient intake forms.
- zHealth’s EHR system features the best chiropractic billing software that allows providers to access a patient’s insurance information with a few clicks.
- zHealth SOAP Note templates and dictation feature allow you to properly document subjective, objective, assessment, and treatment plans.
- The chiropractic insurance billing software by zHealth is ICD-10 compliant. No need to search for CPT codes in a sheet as you can easily create patient statements with a few clicks.
- With zHealth’s automation feature in chiropractic billing software, submit the claims automatically and keep track of your collections.
- zHealth offers the best chiropractic billing services for clinics looking for professionals to handle their claims and billing processes. If you want to see how the best chiropractic billing software helps you save time and money, request a free demo now!
FAQs Related to Chiropractic Medical Billing and Coding
Q: What are the covered chiropractic services under Medicare?
A: Spinal manipulation treatment is a covered service under Medicare. However, Medicare considers only acute and chronic services as active care, and therefore, reimburse chiropractors for these services.
Q: Can I bill for maintenance therapy give to my patients?
A: Medicare only covers acute/corrective treatment to correct acute or chronic subluxation. Medicare does not cover CPT code for chiropractic maintenance.
Q: Do I need to submit a secondary diagnosis during claim submission?
A: Claim submission must include a primary diagnosis of subluxation and a secondary diagnosis reflecting the patient’s neuromusculoskeletal condition. You must document everything related to the services provided to support your claims.
Q: Can I use pain levels to support the acute or chronic category of subluxation?
A: No, you must clearly define the acute or chronic category of subluxation in the patient’s record.
Q: Should I document the effectiveness of the treatment for all subsequent visits for a patient?
Ans: Yes, the documentation must indicate an evaluation of the effectiveness of the treatment provided for all subsequent visits.
Q: Do insurance companies deny claims for chiropractic services based on medical necessity?
A: Insurance companies request chiropractors to send medical records to substantiate the chiropractic services rendered to a patient. If you met the documentation requirements, the claim reviewers send the documentation to a consultant to determine the medical necessity of the services. The insurers can deny claims if they didn’t deem a procedure medically necessary.
Q: How can a subluxation be demonstrated?
A: A subluxation may be demonstrated by an X-Ray or by physical examination.
Q: What is modifier AT and when do I report it?
A: Modifier AT tells us the difference between active treatment and maintenance treatment. When you’re billing Medicare, use AT modifier only when you bill for active/corrective treatment. Claims that do not contain modifier AT will be denied. AT modifier should not be used with CPT code for chiropractic maintenance.
Q: Is there a visit limit for chiropractic services as per Medicare?
A: There is no limit in Medicare for covered chiropractic care services as long as you meet Medicare’s licensure and other requirements.
Q: Is participating and non-participating chiropractors have different documentation requirements?
A: The chiropractic industry has specific documentation requirements. Your participating status nothing to do with documentation requirements. Make sure you stay compliant with HIPAA for maintaining and storing patient data.
Check zHealth Software related FAQs here.
Additional resources:
- https://www.cms.gov/training-education/medicare-learning-network/resources-training
- Medicare Coverage for Chiropractic Services – Medical Record Documentation Requirements for Initial and Subsequent Visits (PDF) MLN Matters Article
- Use of the AT modifier for Chiropractic Billing (New Information Along with Information in MM3449) (PDF) MLN Matters Article
- Educational Resources to Assist Chiropractors with Medicare Billing (PDF) MLN Matters Article
- Medicare Benefit Policy Manual, Chapter 15 (PDF), Sections 30.5 and 240
- Medicare Claims Processing Manual, Chapter 12 (PDF), Section 220
Disclaimer: This is general information about how chiropractic billing company works. Review the chiropractic coverage, requirements, reimbursements, and guidelines of insurance companies by contacting them directly.

